Turning Potential into Performance: A Measurable Investment in MDT Leadership
A White Paper for Commissioners
1. The Gap Between Gold Standard and Operational Reality
Care by a multidisciplinary team (MDT) has long been considered the gold standard for patients with cancer, emphasised since the Calman-Hine report (1995). MDT management is recognised globally as the established model of cancer care, designed to improve decision-making quality, enhance patient-centredness, and reduce variation.
However, growing case complexity and rising patient volumes place increasing strain on MDT time and resources. Without intervention, there is a risk that pressurised meetings deviate from their core purpose, reducing consistency, safety and overall value.
2. The Reality: Critical Gaps in Optimisation and Systemic Risk
While the MDT structure remains correct, inconsistent implementation of national guidance continues to create operational risk and frustration. Feedback from systems across the UK highlights significant gaps in optimisation and behaviour, reinforcing the need for capability-building.
Systemic Barriers to Streamlining and Efficiency
1. Inconsistent Implementation of Streamlining Recommendations
Although the 10 national recommendations exist, implementation remains variable. Feedback across multiple regions highlights the following challenges:
MDT Proformas (Recommendation 1):
A need for fully standardised proformas that include patient preferences, patient understanding, and relevant social issues. Many are incomplete or lack essential information, leading to inefficiency and lost context.
Quoracy and Attendance (Recommendation 6):
Achieving consistent quoracy and regular attendance remains a challenge due to workforce pressures. Some regions aim for 95% quoracy as a benchmark.
Audit and Accountability (Recommendations 8 & 9):
Annual audits comparing treatment decisions to MDT recommendations and consistent mortality and morbidity reviews are not uniformly embedded.
2. Failure to Operationalise Standards of Care (SoCs)
Standards of Care are key to MDT streamlining, enabling non-complex, guideline-aligned cases to bypass routine MDT discussion.
However:
In several tumour groups, every patient continues to be discussed, regardless of complexity.
Clinicians often describe a reluctance to use SoCs, citing a perceived need for all patients to be referred — sometimes described as “defensive medicine” or “rubber stamping”.
Concerns about risk, accountability, or cultural norms often lead to informal overrides of SoCs.
3. Leadership and Resource Constraints: Behavioural and Cultural Barriers
Key constraints affecting MDT efficiency include:
Time Allocation:
Large numbers of low-risk or non-cancer patients continue to be discussed. Observational work shows that more than half of MDT discussions last under two minutes, limiting focus on complex cases.
Clarity of Role:
Some MDT members report uncertainty about their responsibilities, authority, and contribution. Key roles (e.g., Clinical Nurse Specialists) may feel under-empowered despite being primary advocates for the patient voice.
These gaps contribute to duplication, variable decision-making, low psychological safety, and unproductive conflict behaviours.
In a recent publication from the 10 Year Health Plan working group: People, Co-chairs' report it is noted that Clinical leadership and engagement of change will also be vital.
“Clinical leadership must be recognised, developed and supported as a core part of professional practice, with clinicians enabled to lead improvement and transformation alongside their clinical roles, rather than leadership being treated as an optional or additional activity.”
This requires protected time, clear accountability and the development of leadership capability across MDT chairs and core members.
3. The 360° MDT Programme: Turning Potential into Performance
The 360° MDT Programme is a targeted leadership and team-based development intervention that addresses the behavioural, cultural, and process barriers limiting MDT performance. It builds capability to implement national guidance, strengthen governance, and enable measurable improvements.
The programme provides:
Clear ownership and accountability frameworks
Practical leadership tools
Improved chairing and facilitation skills
Behaviourally-focused training to enhance team climate
Structured methods to embed SoCs and agreed pathways
Support to shift MDT culture from compliance to value-creation
Measurable Impact: ROI Through Leadership and System Change
Robust evaluation (Level 1 and 2 data) shows that investing in MDT leadership development creates measurable, sustained improvements.
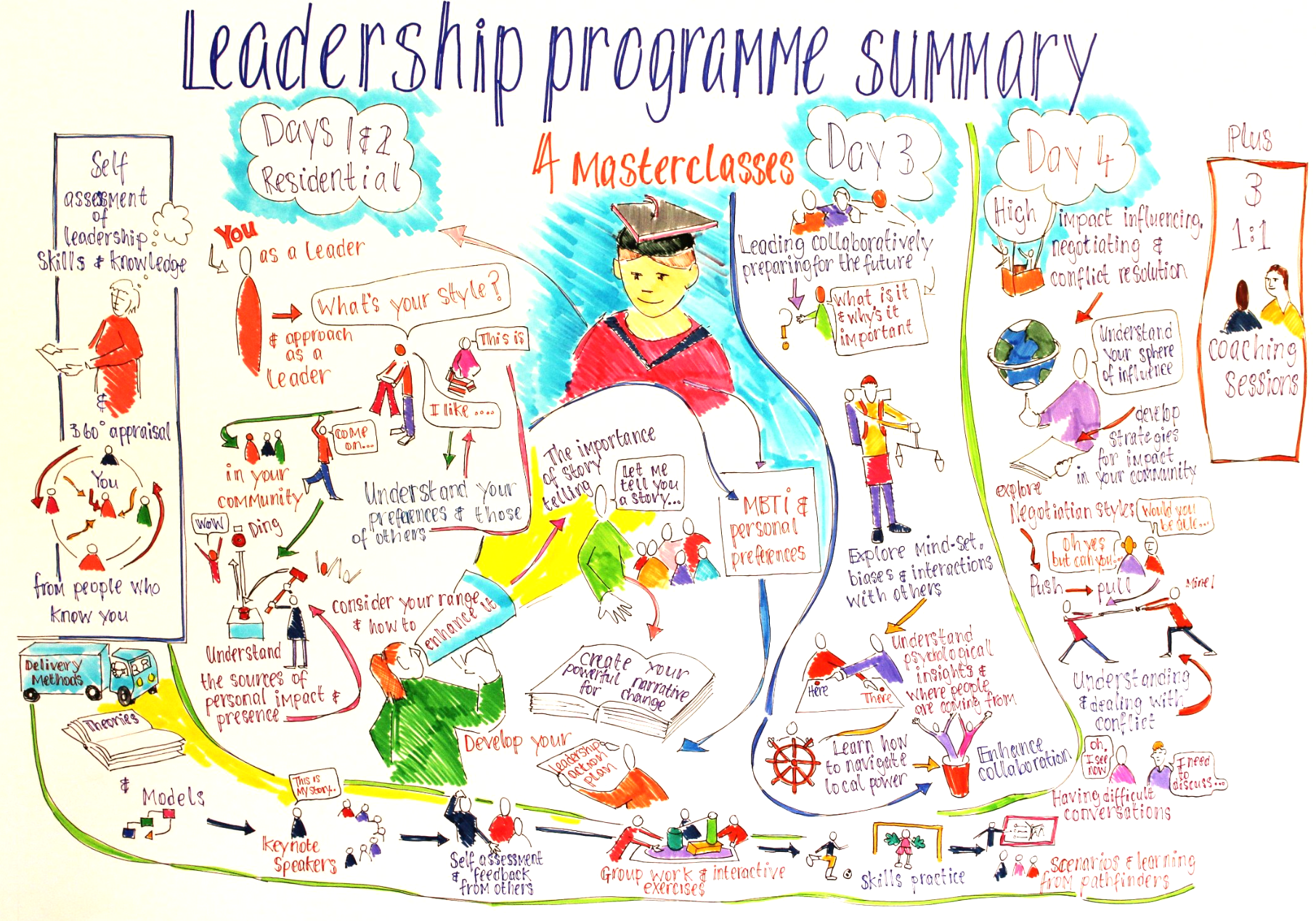
Infographic of performance data
Strengthened Leadership Confidence and Systems Thinking
98–100% of participants gained confidence to lead change.
Over 96% developed a deeper understanding of systemic influences on MDT effectiveness.
Application of systems thinking led to redesigned processes that improved speed and quality of decision-making.
Enhanced Meeting Effectiveness and Chairing Skills
Productivity and timekeeping improved by up to 30% following the introduction of structured frameworks such as the “5 Ps”.
MDT leads reported better structure, reduced disruption, and stronger engagement.
Improved Communication and Emotional Intelligence
90% of participants reported enhanced communication and the ability to apply practical techniques (e.g., regulated pauses, reflective practice).
Improvements in emotional regulation led to better conflict management and more inclusive discussions.
Better Handling of Difficult Conversations
100% of participants reported improved capability and confidence to manage challenging or sensitive conversations.
Use of structured approaches (e.g., Transactional Analysis, OFNR) improved clarity, empathy, and constructive engagement.
Tangible Behavioural and Team-Level Impacts
95–99% of participants committed to changing aspects of how they lead or communicate.
Reported outcomes included higher morale, clearer agendas, improved team participation, and fewer unresolved conflicts.
4. Why Commissioners Should Invest Now
Investment in MDT leadership development is an investment in safe, effective, and efficient cancer care.
Strategic Alignment and Mandate Fulfilment
The programme directly aligns with the NHSE MDT Streamlining Guidance and supports providers to implement sustainable improvements.
Operational Efficiency and Risk Mitigation
By developing leadership capability, the programme supports:
Implementation of Standards of Care
Effective triage and case selection
Reduction of low-value or unnecessary discussions
Increased time for complex, high-risk cases
Improved Patient Flow
Expected outcomes include:
Faster progression along pathways
Reduced delay caused by MDT bottlenecks
Measurable improvement in 62-day and 104-day pathway performance
Sustained ROI
The programme equips MDTs to identify and address system issues themselves, leading to long-term improvements without ongoing external intervention.
Leadership Programme Recap. Image Credit: Matt Worden
5. Conclusion
Multidisciplinary teams remain the correct structure for modern cancer care. However, their intended value is reduced when process, ownership and culture lag behind clinical best practice. The 360° MDT Programme offers a mature, evidence-aligned, and behaviourally grounded approach to improving both MDT performance and patient pathways.
For commissioners seeking improved outcomes, operational efficiency, reduced variation, and alignment with national guidance, this programme represents a proven, high-value investment.